
Decoding the NITI Aayog’s Report on Health System for A New India
In the last couple of decades, has seen noteworthy improvements in the health indicators. The recently released United Nations Development Programme’s Human Development Report (HDI) highlights that India’s gross national income has more than doubled over the last 15 years, from $2,522 (PPP) to $5,497 between 2000 and 2014. This period also registered better human development outcomes; it registered a 0.15 increase from 0.46 to 0.61 between 2000 and 2014.
India has eliminated polio, guinea worm disease, yaws and maternal and neonatal tetanus. Our Total Fertility Rate (TFR) has reduced sharply from 3.4 in 1992-93 to 2.2 in 2015-16. Contrary to expectations, we were able to achieve the Millennium Development Goals (MDGs) in respect of the Maternal Mortality Ratio (MMR level of 130 against a target of 139) and almost succeeded in meeting the Under-5 child mortality target (U5 MR level of 43 against a target of 42).
Continuing and expanding this journey of healthcare transformation is critical to setting up an improved system, which accelerates health outcomes, prevents poverty due to illness and improves the patient’s interface with the health sector.
| By introducing critical health systems transformations, India can: 1. Save more than a million additional children lives and reduce working-age adult deaths by an additional 16% by 2030. 2. Accelerate economic growth. Additional 16% decline in working-age adult mortality would increase real GDP by 64% by 2030. 3. Reduce avoidable out-of-pocket expenses to less than 45%. 4. Will save at least 1.5 million additional households from falling into poverty due to illness. 5. Have a positive impact on the productivity of the working-age population, enabling India to realize its demographic dividend over the next 10-15 years and boosting economic growth. 6. Improve consumer experience and citizen satisfaction and trust in the healthcare system. 7. Grow a globally competitive healthcare insurance and service provision industry with a potentially substantial increase in medical tourism. |
CHALLENGES IN THE HEALTHCARE SECTOR:
The evolution of India’s health system is still a work in progress and there remains a large unfinished agenda. Currently, the Government (Union and the States put together) spends roughly 1.13 per cent of GDP on health, which is grossly inadequate compared to similar spending by other countries. As a result, 62 per cent of healthcare spending is financed by households through out-of-pocket expenditure.
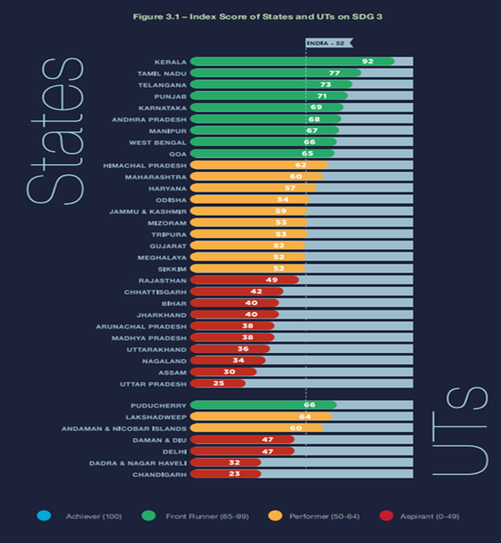
There are significant inter-state and intra-state differentials in health outcomes with socio-economically disadvantaged groups being particularly vulnerable to gaps in access as well as the quality of healthcare available to them.
Further, the Double burden of disease – with a rising burden of non-communicable diseases in addition to the persistence of communicable diseases – stretches the system thin and makes the task of health policymakers all the more complex.
India’s health system reveals a story of multiple fragmentations: a fragmentation of payers and risk pools; deep fragmentation of providers of healthcare services; and also, of the digital backbone running it. This prevents the standardization of purchasing procedures and imposes a huge compliance burden on the providers.
India also suffers from inadequate and fragmented delivery of healthcare services. Over 98 per cent of healthcare facilities in India are those which employ ten persons or less. A consequence of the fragmented provider space is that the health records of patients lie buried in manual systems or in some cases disparate IT systems with little standardization with almost no possibility of inter-operability or cross-sharing, thereby limiting the availability of information that could potentially guide the decisions on health policy.
India also faces the additional challenge of a federal decentralized health policy. Similar to most federal countries, health in India is the primary responsibility of the States. This increases the complexity of avoiding fragmentation of policy formulation and implementation, regulation as well as sector and organization governance.
Severe fragmentation, compounded by market failures and governance challenges, at all levels of the system (financing, service provision, policy formulation, regulation, governance, among others) determines a vicious circle that fuels low performance across all system functions.
STEPS TAKEN BY GOVERNMENT:
The Government of India has initiated the first steps to build a robust health system. Coupled with the strengthening of the public health system under the National Health Mission (NHM), the recent roll-out of Ayushman Bharat — with its twin components of the Health and Wellness Centres to provide comprehensive primary and preventive care at the community level; and the PM Jan Arogya Yojana (PM-JAY) with its Rupee 5 lakh health cover to the bottom 40 per cent of the population.
NITI Aayog’s recent reforms on health sector involves two key components — financing (revenues, risk pooling, and strategic purchasing), as well as organization and provision of health service delivery. Additionally, it also devoted its attention to digital health, which will be a key enabler of system performance.
Successful health sector transformation in India will require reducing funding and provision fragmentation simultaneously This will facilitate effective strategic purchasing, which in turn will determine the incentives for consolidating service providers and improving India’s capacity to enforce much needed patient protection, fair competition, as well as quality and efficiency regulations.
Suggestions on Restructuring the Health Sector in India:
India has a unique opportunity to transform its healthcare system over the next decade or so. Seizing this opportunity requires action and implementation with respect to six pillars of transformation:
1. Further develop and deliver on the unfinished population and public health agenda:
India is in the midst of an epidemiological transition. There is a marked burden of communicable diseases as well as Maternal, New born and Child Health (MNCH) related morbidity and mortality, particularly among the poor.
All these health challenges are amenable to promotive and preventive health interventions, vaccination, contraception, safe delivery, nutritional interventions, infectious disease control, sanitation, clean air and water and health education among others.
The immediate need is to prioritize high-impact and cost-effective interventions at India’s current stage of development — such as finishing the agenda on infectious diseases, which the government should fund fully. The Health & Wellness Centres — with their promise of comprehensive primary care — has to be accorded top most priority and if implemented well, could lay down a solid foundation of our health system.
2. Change health system financing structure away from the predominant undesirable out-of-pocket spending into larger risk pools, with strong strategic purchasing capabilities.
While India may well need to increase its overall level of spending on healthcare, this may not necessarily imply more public resources on health as the only response. The solution lies in improving the performance of the existing risk pools which will better serve beneficiaries as well as reduce wastage of resources. Further, there is need to address the high level of out-of-pocket spending to reduce its negative impact on access to care and poverty as well as to leverage it as a source of additional risk pooling funding.
3. Reduce fragmentation of risk pools and health service provision, incentivizing much needed provider consolidation and organization in networks.
Severe fragmentation in risk pooling hampers the ability of the health system to ensure access to quality, affordable and timely healthcare as well as continuity of care and portability of benefits. It also impedes the ability to set the right incentives for efficiency and long-term sustainability for insurers and healthcare providers.
4. Harness the power of digital health as a critical enabler for the overall transformation of the health system.
Given the fragmented nature of the market, good information systems become even more critical for tracking patients, activity and money, therefore driving efficiency. India requires its own widely accepted data standards, platforms for data exchange across hospital information systems and health insurance information systems.
A powerful IT backbone can also provide real-time information on expenditures, utilization, fraud, quality metrics and drive more value for money for India’s limited health expenditure. Given the IT powerhouse of India, this should be leveraged effectively.
5. Empower patients to become better purchasers of health insurance coverage and health services.
In the dominant out-of-pocket market, the maximum spend is happening for health service provision and purchase of health insurance coverage. Empowering patients to become better purchasers is important for both, purchasing health insurance coverage (when the time comes) and direct purchasing of health services. Consumer information and education plays a critical role here.
6. Implement PM-JAY with an eye on its potential to influence the overall healthcare transformation in India, beyond its current explicit mandate.
The PM Jan Arogya Yojana (PM-JAY) with its Rupee 5 lakh health cover to the bottom 40 per cent of the population for secondary and tertiary care against 1350 odd disease conditions — has laid down a solid foundation on which a good health system can be crafted. It needs to be properly implemented so that services reach the rightful beneficiaries.
CONCLUSIONS: India has a unique opportunity to transform its health sector, which currently lags behind the performance of other comparable economies in the region and worldwide. In doing so, India will not only be able to save millions of lives and avoid millions of households from slipping into poverty due to catastrophic illness but will also further strengthen the virtuous circle of better health and faster economic growth.
Rajesh is Lead Analyst, Strategy & Research, at Indian Political Action Committee. His work and research papers on water contamination, water treatment and soil health have been published in various international journals and conferences.