
7th April is recognized as World Health Day- a day of awareness on various queries regarding healthy living. The World Health Organization (WHO) defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. How does the Indian Healthcare system fare up to this WHO definition? Not very well.
To give a brief background, India has come a long way since Independence from reduction in hunger and malnutrition related issues to becoming a polio-free nation. These feats, as much as they are commendable, are not ends in themselves. The nation now faces a double whammy of communicable diseases like tuberculosis and whopping cough, and non-communicable diseases (NCDs) like those of cardiovascular diseases as a result of changing lifestyles and climate as well as rise in cases of depression, anxiety and other mental health concerns.
Statistically speaking, the health numbers have improved. For example, infant mortality has declined from 74 per 1000 live births in 1994 to 34.6 per 1000 live births in 2016; under-five mortality figure is currently at 41.1 per 1000 as of 2018. But is everything really such a rosy picture? The inter-state as well as the rural-urban inequalities is still glaring- the infant mortality in Kerala is 6 per thousand live births, but in Uttar Pradesh it is 64; the total fertility rate for the country was 2.3 in rural areas whereas it has been 1.8 in urban areas during 2015.
Let us now take the DALY route. DALY or Disability Adjusted Life Years measures the overall burden of disease measured as the years lost due to ill-health or early death. The most common cause of disability adjusted life years lost for Indian citizens as of 2016 for all ages and sexes was ischemic heart disease (accounting for 8.66% of total DALYs), second being chronic obstructive pulmonary disease (accounting for 4.81% of total DALYs), third is diarrhea (accounting for 4.64% of total DALYs) and fourth lower respiratory infections (accounting for 4.35% of total DALYs). One of the most common causes of loss of DALYs for children under 5 years of age was diseases like diarrhea, lower respiratory tract infections and other communicable diseases (accounting for 22,598.71 DALYs per 100,000 population) as of 2016 which are preventable.
Expenditure on Health: A Disappointing Trend.
The nation cannot seem to shake off its name from the list of nations with lowest expenditures on healthcare. The WHO’s health financing report of 2017 states that about 68% of health expenditures in India is done out of pocket while the global average is around 12%. In fact, the OOP expenditures pushes a good fraction of the population towards poverty and sometimes, even below the poverty line.
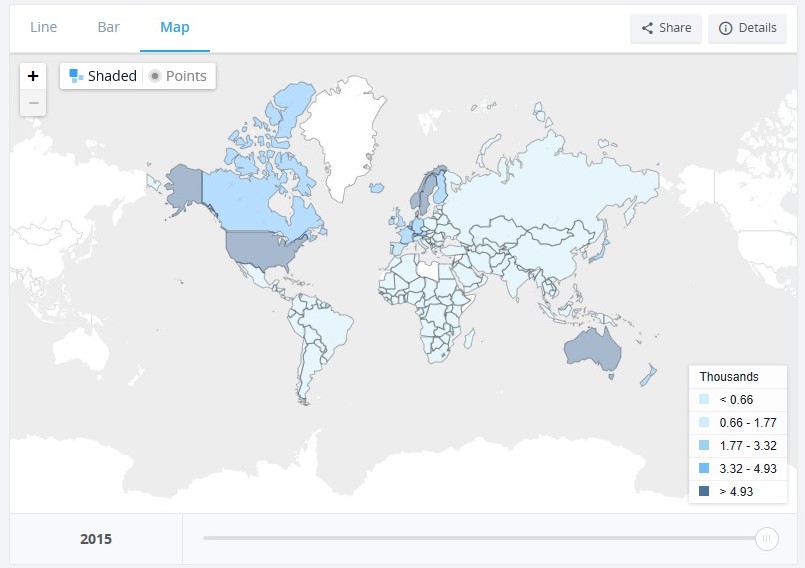
According to the World Bank, India spent 4.18% of her GDP on the health sector in 2000 which dropped to 3.89% in 2015. The global average, however, increased from 8.6% to 9.9% in the same period. The per capita health expenditure, PPP (current international $) increased from 18.56 in 2000 to 63.32 in 2015. The following images give the global perspective:

Source- The World Bank.
Source- The World Bank.
Ailing Primary Health and Infrastructural Issues.
The foundation of the Indian Healthcare hierarchy is definitely not in a great shape. The primary healthcare centres (PHCs), the supposedly first line of health service and emergency provisioning, lies in neglect. There are reports of lack of basic medicines and negligible manpower to lower levels of accessibility. There might be a PHC in the vicinity but the road connecting it is in tatters or too narrow for an ambulance to pass through. Ground reports can give a much detailed picture but unfortunately, the mainstream media has a very different set of priorities.
Doctors and medical staff are low in comparison to the number of patients in public hospitals. In economic terms, there is a very low physician density in the catchment area. The implications are quite unhealthy- with absentee doctors, the pressure to handle a vast number of patients fall on interns who are not equipped yet to deal with critical and complicated cases. The recent spike in violence against doctors and medical professionals could be partly attributed to this low physician density.
The Booming Private Sector.
What is essentially supposed to be a subsidized service provided by the state, health service is largely getting transformed into a booming profit-making enterprise. The pathetic conditions in most public hospitals give an undue advantage to the private players in the sector, who are charging exorbitantly for health services. The population is also changing gears towards private hospitals in hope of quality services, despite the high pricing system. The implication being medical poverty as not much of the population is covered by insurance.
It is interesting, however, that in all of this confusion, quality health services are essentially becoming an auction- pay more to get the best.
Final Thoughts.
There could be much more that could be written on the subject. Health, being a state subject in the Indian Constitution, the policies differs according to the concerned state’s peculiarities but the primary demand is similar- access to quality health services which includes emergency care, maternity care, child care and everything in between. There is an immediate call to increase public health expenditure, improve the deteriorating infrastructural conditions across the hierarchy while improving access to medical centers, starting at the PHC level. While the middle and upper-middle classes might be able to afford private healthcare services, the poor and the poorest of the poor need and want the public sector. Ending this with a line I had read in my health economics course:
Health is not everything in life, but without health, life is nothing.
Calcutta University.