
(This is second in a series of two articles)
Health is understood as a subject of ‘Market Failure’. But because it is the subject of social welfare there is need of an intermediary mechanism for active intervention. One such important mechanism would be regulation. In order to maintain and ensure quality healthcare and equitable allocation of resources now it is well addressed or considered of the need of regulation. Regulation is defined as “actions by government bodies and government-appointed regulatory agencies to influence the provision of health services and health insurance by private providers” (Mckintosh 2007). Actually it is a narrow definition of regulation because it does not include the non-state actors in the regulatory action. So the broader definition would be: “a diverse set of actions and arrangements undertaken by a range of state and non-state actors, to control and modify individual and organizational activity in the field of health care provision” (McPake & Mills, 2000).The irrational and unregulated nature of the private sector in India is well documented (Baru, R 2013; Bhat, R 1996). There are some important issues related to health for which regulation is necessary. These issues are:
- Medical Negligence cases: There is enough evidence to prove the medical negligence in India.Horrible Negligence! 4-Month-Old Baby Given Painkillers, Dies Within An Hour At Delhi Hospital.[1]
- Overcharging by hospitals: There is enough cases against the private players in health services for overcharging. The Fortis hospital charged Jayant Singh nearly Rs 16 lakh for the treatment of his seven-year-old daughter, who died of dengue.[2]
- Reduction in inequality (Decrease in OOPE, gender, class, social stigma and caste gaps ) : To save people from poverty by decreasing OOPE which has also some intrinsic value like discrimination and empowerment. Out-of-pocket (OOP) health expenses drove 55 million Indians – more than the population of South Korea, Spain or Kenya – into poverty in 2017, and of these, 38 million (69 percent) were impoverished by expenditure on medicines alone.[3]
- Organ transplant scams: This has become a millionaire business in the India.Several private hospitals in Tamil Nadu’s Chennai may be unfairly favouring foreign transplant recipients over Indian patients on waiting lists for organs.In 2017, international patients underwent 25% of all heart transplants in the state and 33% of lung transplants in Chennai.[4]
- Referral commissions to Physicians: The physicians/doctors are paid the commissions for the referrals to the diagnostics or any specific medicine.
- To get lands from government at concessional/low rates in lieu of free or low cost services for BPL: The Delhi High Court has indicted a private hospital for not following the rules (High Court of Delhi ruling no 2866/2002). Because there are violations found at many places.
- Late in providing cash maternity benefits: The maternity benefit scheme in Delhi called MAMTA scheme instituted by Delhi government for institutional deliveries in private sector also was a failure ostensibly for the reason that the private providers found it to be not very ‘remunerative’ (Nandan et al 2009). In Karnataka there is enough evidence to show that PPP based health care system use to provide late maternity benefits.
- Untrained or unqualified doctors: Unqualified medics, popularly known as quacks, are routinely arrested in India for posing as doctors. But a charity is now trying to train them in primary medical care. [5] But in other cases they are responsible for many deaths in India because of the work which they are not supposed to do.
6. Regulatory Architecture and gaps in healthcare in India
Health is a subject of state in India. Therefore, states use to play vital role in shaping the delivery of health services. Therefore, states can bring in specific regulatory mechanisms to influence private/public sector behavior. The union governments and states governments use to bring in monitoring and regulatory mechanisms time to time. For instance, Clinical Establishments (CE) Act and its earlier variants the various state nursing home (NH) acts for licensing and registrations of CE; Medical council Act for the licensing of medical practitioners; Medical termination of Pregnancy Act (MTP) and so on.
Clinical Establishment (Registration and Regulation) Act(CEA) was passed in 2012. The union government passed this act as prototype which each state has to customize accordingly. In this act there is provision of making national and state level health council. Various inspections of the facility for adherence of the standard set by NHPS.Another provision was the penalties for non-compliance. But only 16 states adopted it. Some other states have their own previous NHP act or acts with some amendment subsequently. But Gujarat state does not have any regulation act. Only Chhattisgarh state adopted CEA which includes patient’s right and grievance redressal mechanism. Whereas Bihar has adopted it without any change, as we know that every state/region have its own cultural, social and political scenario and they should change it accordingly so that it can be make implementable. It mean health is the subject of decentralization for effective and better outcome.
Another act is Medical council of India Act which was passed in 1956 but revised in 1964, 1993 and 2001. This act prohibits physicians from taking any gifts. By the provisions of this act physicians should only provide prescribed generic medicines. They should declare all fee before the procedures being started. They should follow proper referral procedures. Endorsement of any drug from the industry is not permitted. Any professional misconduct would be taken into the concern of state medical councils for appropriate disciplinary action.
In the Medical Termination of Pregnancy Act provides legal termination of pregnancy by a registered medical practitioner and there should not be any sex selection test. In the Transplantation of Human Organ Act, 1994 there is the provision that organ transplantation can be done only by legal completing legal formalities among blood related persons.
7. Recommendations: Proposed Regulatory Architecture for regulation of private sector
One of the most important command and control mechanism is through judicial process like consumer courts. “Contracting-out of non-clinical services could be considered in a Universal health system, where non-clinical services such as laundry, security, maintenance, kitchen and dietary services are given to private contractors under well-defined legal agreements that uphold
quality, place restriction charges with penalties if violated, and are accountable within a universal access framework. A small evaluation study in Bihar found that hospital upkeep had improved post outsourcing” (Gupta M,S. Prasanna undated). Right to health should be in the mind of policy makers while framing regulatory mechanism for healthcare services. Intersectoral approach would be more beneficial for integrated public health model for good, efficient and effective outcome. Establishment of quasi-judicial-authoritative regulatory body is necessary to be form for grievance redressal, it should have ample staffs, finance and infrastructure. Public health systems should bring ‘monopsony’ power to endure on the private players to drive for both high quality and low costs.
Way Forward
In India there is the strong need of ‘Right to Health Care Legislation’. There should also be an autonomous quasi-judicial authoritative regulatory body. This proposed body should be well financed and good number of staffs. Under the ministry of health. There is also strong need to strengthen the public health system by financing, integrating some other institutions, universal , signal system. Markets usually function optimally where public system is strong. “The PFHI (Publicly Financed Health Insurance) schemes at present are not universal but targeted, fragmented and sometimes multiple schemes catering to the same population run by different ministries resulting in efficiency losses” (S.Prasanna, 2018). There is also need of strong and reasonable standard. Because the the process by which regulation use to be introduced may be the subject of potential root cause for corruption, red tape, harassment in the country like India where judicial processes are very slow.
Hence it becomes very important that reasonable standards with the involvement of all stakeholders are set; information disseminated; facilitating compliance and minimizing the scope for corruption (Das Gupta M, et. al. 2009).
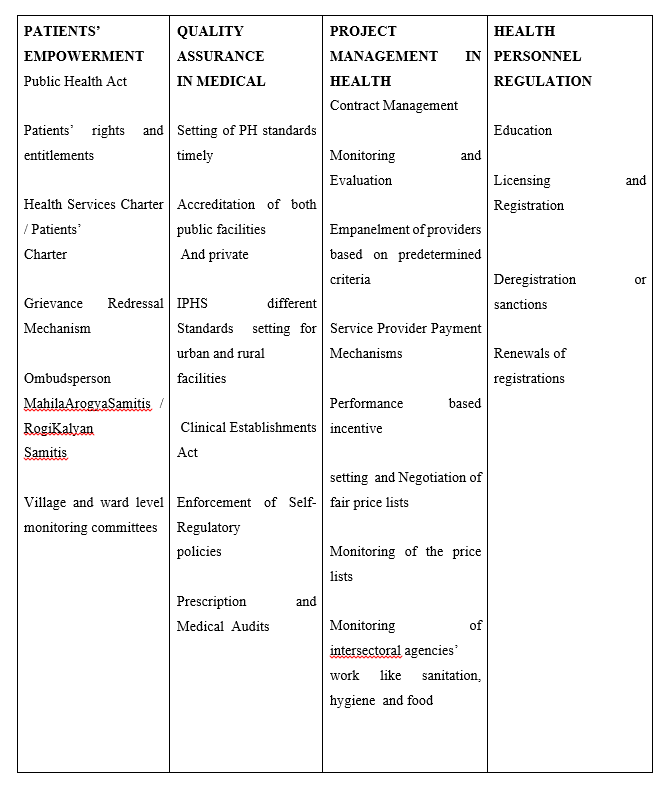
So, the proposed regulatory mechanism would be in four sector at three levels of nation, state and district.
[1] https://www.indiatimes.com/news/india/horrible-negligence-4-month-old-baby-given-painkillers-dies-within-an-hour-at-delhi-hospital-338039.html
[2] https://economictimes.indiatimes.com/industry/healthcare/biotech/fortis-healthcare-refutes-charges-of-over-pricing-drugs/articleshow/62095787.cms
[3] https://www.firstpost.com/india/indias-healthcare-woes-out-of-pocket-medical-expenses-pushed-55-million-into-poverty-in-2017-says-phfi-study-4773741.html
[4] https://scroll.in/latest/882307/chennai-private-hospitals-favour-foreigners-over-indian-patients-for-organ-transplants-says-report
[5] https://www.bbc.com/news/world-asia-india-37571259
References:-
- Samb, B., Desai, N., Nishtar, S., Mendis, S., Bekedam, H., Wright, A., … & Adshead, F. (2010). Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. The Lancet, 376(9754), 1785-1797.
- Horng, J. S., Liu, C. H., Chou, H. Y., & Tsai, C. Y. (2012). Understanding the impact of culinary brand equity and destination familiarity on travel intentions. Tourism management, 33(4), 815-824.
- (National Health Accounts, https://mohfw.gov.in/sites/default/files/National%20Health%20Accounts%20Estimates%20R
- eport%202014-15.pdf )
- Reddy, K. S., Selvaraj, S., Rao, K. D., Chokshi, M., Kumar, P., Arora, V., … & Ganguly, I. (2011). A critical assessment of the existing health insurance models in India. Public Health Foundation of India, 4, 1-15.
- Sheikh, K., Saligram, P. S., & Hort, K. (2013). What explains regulatory failure? Analysing the architecture of health care regulation in two Indian states. Health policy and planning, 30(1), 39-55.
- Välilä, T. (2005). How expensive are cost savings? On the economics of public-private partnerships. EIB papers, 10(1), 95-119.
- Hay, D. A., & Morris, D. J. (1991). Industrial economics and organization: theory and evidence. Oxford University Press, USA.
- Nundy, Samiran, Keshav Desiraju, and Sanjay Nagral. Healers or Predators?: Healthcare Corruption in India. Oxford University Press, 2018.
- Laurell, A. C. (2007). Health system reform in Mexico: a critical review. International Journal of Health Services, 37(3), 515-535.
- Martens, J. (2007). Multistakeholder partnerships-future models of multilateralism? (Vol. 29). Berlin: Friedrich-Ebert-Stiftung.
- Gilson, L., Doherty, J., Loewenson, R., & Francis, V. (2007). Challenging inequity through health systems. Final report of the Knowledge Network on health systems.
- McPake, B., & Mills, A. (2000). What can we learn from international comparisons of health systems and health system reform?. Bulletin of the World Health Organization, 78, 811-820.
- Baru, R. V. (2013). Challenges for regulating the private health services in India for achieving universal health care. Indian journal of public health, 57(4), 208.
- Bhat, R. (1996). Regulation of the private health sector in India. The International journal of health planning and management, 11(3), 253-274.
- https://economictimes.indiatimes.com/industry/healthcare/biotech/fortis-healthcare-refutes-charges-of-over-pricing-drugs/articleshow/62095787.cms
- https://www.news18.com/news/india/httpwww-news18-comnewsindiagurugram-hospital-charges-rs-18-lakh-for-15-day-dengue-treatment-girl-dies-1582807-html-1582807.html
- https://www.firstpost.com/india/indias-healthcare-woes-out-of-pocket-medical-expenses-pushed-55-million-into-poverty-in-2017-says-phfi-study-4773741.html
- https://scroll.in/latest/882307/chennai-private-hospitals-favour-foreigners-over-indian-patients-for-organ-transplants-says-report
- https://www.bbc.com/news/world-asia-india-37571259
- Gupta, M. S. (2000). Corruption and the provision of health care and education services. International Monetary Fund.
- Varghese, J., Blankenhorn, A., Saligram, P., Porter, J., & Sheikh, K. (2018). Setting the agenda for nurse leadership in India: what is missing. International journal for equity in health, 17(1), 98.
- Gupta, M. D., Chung, W., & Shuzhuo, L. (2009). Evidence for an incipient decline in numbers of missing girls in China and India. Population and Development Review, 35(2), 401-416.
Vikash Prakash studied M.A Development (Public Health) at Azim Premji University, Bangalore. He is a Young Professional working with StartUp Incubation and Innovation Center, IIT Kanpur.