
In India, government health expenditure has stayed between 1.1-1.4% of the GDP over the last decade1. Out-of-pocket health expenses pushed about 55 million Indians into poverty, and 38 million of them fell below the poverty line due to spending on medicines alone2,3. The poverty trap of health expenditures demands a severe and urgent revamping of the healthcare payment system. The usual models of healthcare payment are fee-for-service (a patient pays a specific price for each service), payment by an episode of illness (making the payment for all services provided during one visit or one hospital stay), per diem payment (making payment for all the services provided in one day), salary (making a fixed payment that contributes to clinicians’ income for predetermined working hours) and global payment (making a fixed payment to hospitals for all services given to a patient for a specified period, usually a year)4.
An alternate avenue is the emerging value-based health care (VBHC) model. It emerged with the need for creating “continuously learning healthcare systems”5 that allow the best treatments while emphasizing patient-centered care and openly seeking patient preferences and input. It is a healthcare delivery model in which providers are paid based on patient health outcomes6. It focuses on what patients value and allocates resources according to the health outcomes delivered by the system7. As put by Dr. Robert Nesse, a healthcare reform researcher, “What would the cost of a hamburger be if, instead of paying for the outcome of good food delivered in a suitable location by friendly service, we actually just paid for the number of cooks and wait staff? The economics of health care are not dramatically different from this. We currently pay for the process and not the outcome8.”
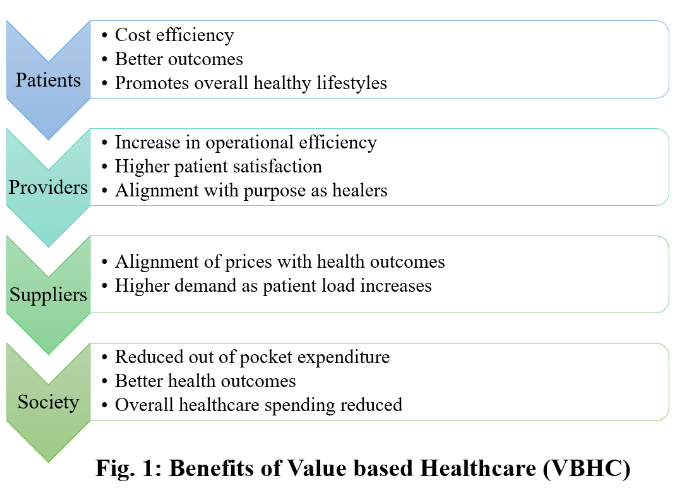
In VBHC, growth in revenue is not tied to the number of services provided per patient but to the quality, safety, patient experience, and participation in decision-making. It creates motivation to eliminate unnecessary diagnostic and therapeutic interventions, promoting cost-saving while still being compliant with evidence-based guidelines. In comparison, in the traditional fee-for-service model, every consultation, test, or procedure is paid-for regardless of its need and outcomes. The benefits of a value-based healthcare system extend to patients, providers, payers, suppliers, and the broader society (Figure 1)6.
Various value-based healthcare pilots like Accountable Care Organisation, Value Institute for Health and Care, Avant-garde Health, American College of Surgeons’ THRIVE (Transforming Health care Resources to Increase Value and Efficiency) Initiative, etc. have been undertaken in developed countries demonstrating promising results6,9. In India, conditions that call for VBHC include a large uninsured population, severe shortage of doctors and facilities, and lack of rigorous regulations. The challenge in India is to deliver a high volume of quality medical services at affordable low costs requiring breakthrough in healthcare delivery10. A few Indian hospitals pioneering VBHC, Narayana health11, Aravind Eyecare12, LV Prasad Eye Institute, Care Hospital13, Deccan Hospital14, HCG Oncology15, LifeSpring Hospital16, and Muktangan17 have had considerable success. To deliver on their dual commitment to the high quality of care and low costs, they have developed mechanisms like a hub-and-spoke configuration of assets (a tertiary hub for specialized procedures and primary ‘spoke’ centers for smaller interventions), innovative task-shifting approaches, and a focus on the cost-effectiveness of procedures rather than just cost-cutting18.
An even more innovative small-scale pilot in a Mumbai suburb has taken the notion of ‘value’ a step further. ‘Prerna Prakalp – pay as you value clinic’19, started by Dr. Sushant Shinde in September 2019, aims to place the value of health services provided in the patients’ hands. The clinic, backed by a charitable organization, lets its patients determine the value of payments for the services (consultations and tests) and medications that they receive. Patients can pay a part or total cost, according to the ‘perceived value’ of the services provided to them. The rest of the amount is matched up by the trust funds. The primary goal of the venture is to provide the patient with the choice of the amount that they are willing to pay. This goes in line with the health economics research depicting the importance of willing-to-pay for determining cost-effectiveness in the context of health outcomes20. It also helps relieve the care provider-patient relationship from the stress of overt financial calculations. Towards the funding side, Prerna plans on modifying the role of charitable organizations from ‘grant-giving’ to ‘contributing’. As per Dr. Shinde, Prerna Prakalp has had encouraging support in the first six months of establishment, with more than 42% of patients paying more than or equal to the actual costs incurred to the clinic. These numbers will become more reliable, with more patient volume over time.
VBHC has been attempted in other countries for multi-disciplinary tertiary level hospitals 21,22. However, small-scale implementation of VBHC under private practitioners, like Prerna Prakalp, is essential for grass-roots expansion23. The VBHC model is an avenue for private healthcare providers who wish to contribute to society without engaging in corporate hospitals’ politics or purposeless profiteering. From Prerna Prakalp’s experience and growing global literature, it seems that the ‘pay as you value’ approach could function for high-cost procedures in surgical24 and critical-care setups too.25 When the patient has the option of zero payment, there is an obvious concern about undervaluing particularly for outpatient services. However, this is not true for surgical and critical care where ‘life-saving’ procedures and services are inherently valued more.
Hence, generally, VBHC ensures that the interests of the patients and practitioners are aligned; the healthcare practitioner is incentivized to focus on the quality and safety of care, and patients’ satisfaction and vocal participation, instead of prescribing countless procedures and the patients are motivated (or positively forced) to make such a healthcare system sustainable. VBHC initiatives come in with quadruple aims: better patient outcomes, improved patient experience, improved staff satisfaction, and lower cost of health care7,26. They can connect clinicians to their purpose as healers, support their professionalism, reduce burnout, and align them with their patients’ better health27.
References:
1. Bhattacharya S. Role of private sector towards universal health coverage in India. Published May 6, 2020. Accessed August 22, 2020. https://timesofindia.indiatimes.com/blogs/voices/role-of-private-sector-towards-universal-health-coverage-in-india/
2. Public Health Foundation of India. Accessed August 22, 2020. https://phfi.org/
3. Rao N. Who is paying for India’s healthcare. The Wire, April. 2018;14. https://thewire.in/health/who-is-paying-for-indias-healthcare
4. Vineet Arora & Christopher Moriates & Neel Shah – Understanding Value Based Healthcare.pdf.
5. Smith M, Saunders R, Stuckhardt L, Michael McGinnis J, Committee on the Learning Health Care System, Institute of Medicine. A Continuously Learning Health Care System. National Academies Press (US); 2013. Accessed August 24, 2020. https://www.ncbi.nlm.nih.gov/books/NBK207218/
6. null null. What Is Value-Based Healthcare? Catalyst Carryover. 3(1). doi:10.1056/CAT.17.0558
7. Here’s how to make “value-based healthcare” a reality. Accessed August 23, 2020. https://www.weforum.org/agenda/2019/02/here-s-how-to-make-value-based-healthcare-a-reality/
8. Smoldt RK, Cortese DA. Pay-for-performance or pay for value? Mayo Clin Proc. 2007;82(2):210-213. doi:10.4065/82.2.210
9. Value-Based Health Care – Institute For Strategy And Competitiveness – Harvard Business School. Accessed August 23, 2020. https://www.isc.hbs.edu/health-care/value-based-health-care/Pages/default.aspx
10. Sengupta H. India has a lot to teach America in healthcare: Vijay Govindarajan. Fortune India. Published July 2, 2018. Accessed August 23, 2020. https://www.fortuneindia.com/people/india-has-a-lot-to-teach-america-in-healthcare-vijay-govindarajan/102075
11. Narayana Health. Accessed August 22, 2020. https://www.narayanahealth.org/
12. Home – Aravind Eye Care System Aravind Eye Care System. Accessed August 22, 2020. https://aravind.org/
13. The Story of CARE – Care Hospitals. Accessed August 23, 2020. https://carehospitals.com/about-care/the-story-of-care/
14. Best Orthopaedic Hospital in Pune. Accessed August 23, 2020. http://deccanhospital.in/
15. Best Cancer Hospital in India. Accessed August 23, 2020. https://www.hcgoncology.com/
16. Johar G. LifeSpring hospitals. Columbia Business School. Published online 2010. http://www.lifespring.in/
17. Home. Accessed August 22, 2020. https://www.muktangan.org/
18. Govindarajan V, Ramamurti R. Delivering World-Class Health Care, Affordably. Harvard Business Review. Published online November 1, 2013. Accessed August 23, 2020. https://hbr.org/2013/11/delivering-world-class-health-care-affordably
19. Prerna Prakalp – Pay As You Value Clinic.; 2019. Accessed August 23, 2020. https://youtu.be/sfChe8UGpqI
20. Nimdet K, Chaiyakunapruk N, Vichansavakul K, Ngorsuraches S. A systematic review of studies eliciting willingness-to-pay per quality-adjusted life year: does it justify CE threshold? PLoS One. 2015;10(4):e0122760. doi:10.1371/journal.pone.0122760
21. A Shift to Value-Based Healthcare. Published March 1, 2017. Accessed August 23, 2020. https://healthinformatics.uic.edu/blog/shift-from-volume-based-care-to-value-based-care/
22. How and why value based purchasing is trending in the healthcare industry. Published June 28, 2019. Accessed August 23, 2020. https://www.businessinsider.in/science/how-and-why-value-based-purchasing-is-trending-in-the-healthcare-industry/articleshow/69981972.cms
23. Teisberg EO, Wallace S. Creating a high-value delivery system for health care. Semin Thorac Cardiovasc Surg. 2009;21(1):35-42. doi:10.1053/j.semtcvs.2009.03.003
24. Blasco T. Successful Implementation of Value-Based Surgical Care Using Comprehensive Analytics. Accessed August 24, 2020. https://blog.surgicaldirections.com/successful-implementation-of-value-based-surgical-care-using-comprehensive-analytics
25. O’Brien JM Jr, Kumar A, Metersky ML. Does value-based purchasing enhance quality of care and patient outcomes in the ICU? Crit Care Clin. 2013;29(1):91-112. doi:10.1016/j.ccc.2012.10.002
26. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff . 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759
27. Teisberg E, Wallace S, O’Hara S. Defining and Implementing Value-Based Health Care: A Strategic Framework. Acad Med. 2020;95(5):682-685. doi:10.1097/ACM.0000000000003122

This article has been co-authored by Jeel Vasa, Siddhesh Zadey and Rachit Sekhrajka.
Acknowledgments: We thank Dr. Sushant Shinde, founder of Prerna Prakalp, for sharing the details about his venture and allowing their use for this article. We would also like to thank Dr. Sweta Dubey for her critical feedback.
Siddhesh Zadey is a graduate student at the Duke Global Health Institute, Duke University, Durham, North Carolina, United States. Jeel Vasa and Rachit Sekhrajka are currently MBBS students.All authors work with the Indian non-profit research group ASAR.